If you think of preparation for labour as a recipe, as Women’s Health therapists we would like to add some ingredients. Good preparation is key and we hope the following advice will help with your prenatal care. We’ve also added a couple of tips for birth and beyond.
- During pregnancy and after your 12-week scan, you should visit a Women’s Health Specialist to assess whether you are doing your pelvic floor contractions correctly. This is essential especially helpful if you have any pelvic girdle or back pain, urinary leakage, consitpation or vaginal heavyness. We will also give you guidance and advice on how to reduce the risk of pelvic floor trauma during labour, good factual information will support you before, during and after labour.
-
After your assessment, continue with your pelvic floor exercises (an individual program will be set up by our women’s health team) up until 35/36 weeks. It is important to focus on the release phase of the pelvic floor contraction, so you are not building tension in the muscle.
- At 35/36 weeks, we would recommend that you stop your pelvic floor exercises and start perineal massage. See our team if you are unsure or not confident enough to perform and then you can continue at home on your own or with your partner (or in the clinic if you are not comfortable doing self-release work)
- It is important to trust yourself and engage in your own labour. Have a clear birth plan and know what you do/don’t want even if labour does not go to plan. The more you know, the more educated your decisions can be.
- Add ‘How to Have A Baby’ by Natalie Meddings to your reading list. This book is fully equipped with everything you need to know about childbirth preparation and top tips on how to prepare yourself. Your hospital bag isn’t just for when you’re in hospital, we would encourage you to create a ‘kit bag’ for when you’re at home and in labour. Knowing that you have everything you need within reach can be a real comfort; There is a tried and tested list in Natalie’s book. Make the kit bag your own and ‘having it there’ will help your sense of privacy, warmth, safety and quiet.
- Following delivery- ice, elevate and rest your pelvis. Check the catheter regularly and ensure it does not get too full. Prevent constipation- go on urge, support your perineum, and keep up a high fibre diet. We would recommend adding psyllium husk or ground flax seed (diluted in your breakfast) to your diet.
- Post-natally, do not do strong pelvic floor exercises until it feels comfortable. Allow any stitches to heal first. You can perform gentle contractions for circulation, increase the contraction hold time based on you babies age in weeks (eg 1 sec hold for 1 week old, 2 sec hold for 2 weeks old etc.)
- Prioritise your own recovery, 6 weeks post-delivery, we would encourage all mums to come and have a Post-natal MOT (C-S or NVD.) Your clinician will do a full internal and external assessment and work with you to plan your return to exercise, check your pelvic floor, check your abdominal wall, and set up an individualised program as well as assessing your risk profile. We will guide you to return to all the activities you enjoyed before being a mum.
Tracey and Fara are our pre & postnatal specialist, and are looking forward to meeting you.
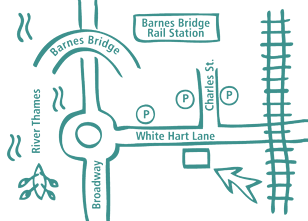
Our Barnes Clinic
Our clinic is located in Barnes, South-West London and is easily accessible by public transport.
For more information including parking and other practicalities see our Barnes clinic page
Book an Appointment
Booking an appointment with one of our therapists is quick and easy. There is no long waiting time and you don’t need a referral from your GP.