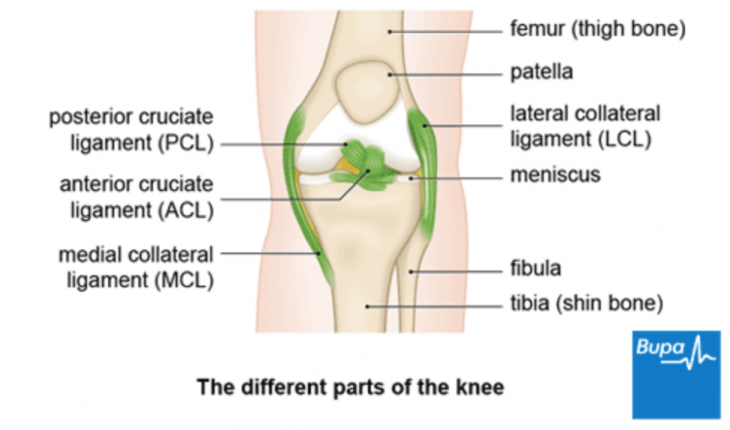
ACL reconstruction is a very common surgery to repair a ruptured ACL. Traditionally, rehabilitation and process to return to sport has been predominantly time based. Meaning at certain points post op, rehab was progressed. However, with literature reports re-rupture rates on the operated leg from 6-25% (Simon et al, 2005), and the opposite leg ranging from 2-20% (Walden et al 2006, Wright et al, 2007) it became evident time since surgery alone is not enough to ensure safe return to sport.
As a result, the way we approach ACL rehab is changing. The Melbourne ACL Guideline has been developed by Mick Hughes and Randall Cooper in Australia. These guidelines describe ‘criterion-based progression.’ This concept builds on time since surgery by ensuring the individual ticks off criteria relating to strength, balance, function, swelling and pain, as well as confidence. This allows safe progression through increasing demands of rehab and eventually return to sport. Meeting these criteria are crucial for return to , with recent evidence indicating a four times increased risk of re-rupture if discharge criteria are not met (Kyritsis et al. 2016).
This blog is designed to educate you about these guidelines to help set realistic expectations, and how you can access these with us to assist with your rehabilitation.
Finally, recovery from an ACL injury is an individual journey. Factors such as, but not limited to your fitness level, surgery type and physical demands of your sport can dictate your exercise programs. As such, basic exercise ideas are presented but not a structured program. This is something we develop with you and your sports medicine team to ensure optimal results.
Rehabilitation Milestones
Phase 1: Getting things going
Initial recovery from surgery can be tough as you’ll likely feel tired and sore. Pain and swelling will be at its peak. Overall though, you will continue to improve a bit each day. Your goals are:
- Reduce swelling as much as you can.
- Achieve full extension a few weeks after surgery
- 0 quadriceps lag
- Normal walking pattern
Basic quad activation, range of motion exercises and walking practice are key exercises here.
Phase 2: Strength, strength, strength
Aims here are to restore as much single leg balance and strength between sides as possible. Maximising strength protects the graft and allows safe return to running/jumping while minimising risk of developing other types of pain. During this phase we focus on double and single leg exercises e.g. squat, lunge for the whole lower limb. With emphasis on slow movement and proper form with each exercise. During this phase Listen to your knee. Increased pain and swelling are signs the knee is not coping. We will help you manage this in collaboration with your coaching staff. We progress through closed kinetic change and open kinetic chain exercises.
- Leg extensions and open kinetic chain exercises? This is a topic of hot debate. Recent research has these exercises can be safe within 90-45degrees of knee flexion in the first 2 months (Perriman et al, 2018). However, we always discuss these with your surgeon first.
- Graft healing: This phase includes weeks 6-12 post op. During this time the graft is at its weakest point as the original tendon changes structure into a ligament. This process is called religamentisation. It’s very important that no running or jumping is performed during these weeks.
Milestones
- Full Extension
- Full flexion
- Nil swelling
- Equal single leg balance
- Equal maximum repetitions between sides for single leg bridge, calf raise, side bridge
- Good lower limb alignment during single leg squat to at least 60 degrees and 85% maximum repetitions between sides.
Although these next goals may not be achievable right now, you should work towards these over the course of your rehab:
- Single leg leg press 1RM 1.5x body weight
- Squat 1RM 1.5x body weight
Phase 3: Hopping, running and agility
With appropriate strength and approval from your specialist (usually about 4 months post op), we can commence plyometrics (hopping), straight line running, followed by change of direction and agility work. Field training is very important for this for physical rehab but also improving your confidence with running and change of direction. With this phase of rehab loads on your knees, ankles and hips are increase substantially due to increased volume, and higher energy required for running, jumping etc. Due to this the risk of developing other sources of pain such as patellofemoral pain, tendinopathy, and bone stress injuries is higher. We will work closely with your coaching staff to monitor this. During this time, strength training continues.
When can I return to running?
- Once you have achieved the milestones of phase two
- Achieve >85% scores on dynamic hopping tests between sides.
Milestones
- Pain free knee with no swelling
- Complete running/agility program
- Complete full field training
- Ensure equal single leg strength and hopping performance
Try to increase your strength as well!
- Single leg leg press 1RM 1.8x body weight OR
- Squat 1RM 1.8x body weight
Phase 4: Return to sport
Current research supports return no earlier than 6 months post op, with risk of re-rupture reduced by 50% for every month delayed until 9 months. Return to sport is a team decision, based on your surgeons guidance, your confidence level, and criteria for return to sport. Times will vary also based on the physical demands of your sport. Those that do not require, jumping, and pivoting may permit earlier return than those that do.
Return to sport criteria:
- 90% symmetry for lower limb strength, balance and hopping tests
- Completed training at full intensity
- Psychologically ready – there are self-assessment surveys to help with this.
When return to sport has been achieved, the greatest challenge is prevention of re-rupture. Continuation of your exercise program is crucial. It is not longer a rehab program but a maintenance/prevention program. The Fifa 11+ injury prevention program is also very useful.
Thank you for reading this, we hope you found it informative! If you have sustained an ACL injury, you can subscribe to the Melbourne ACL Guide. It is de-identified and free. You can then give us access to work with you to track your progress over the course of your rehabilitation.
Visit our Physiotherapy page for more information about the service at the clinic.
References:
Perriman, A., Leahy, E., Semciw, A. I. (2018). The Effect of Open- Versus Closed-Kinetic-Chain Exercises on Anterior Tibial Laxity, Strength, and Function Following Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Journal of Orthopaedic & Sports Physical Therapy. 48(7). 552-566
Salmon L, Russell V, Musgrove T, et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948–57.
Waldén M, Hägglund M, Ekstrand J. High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br J Sports Med 2006;40:158–62.
Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med 2007;35:1131–4.
Our Barnes Clinic
Our clinic is located in Barnes, South-West London and is easily accessible by public transport.
For more information including parking and other practicalities see our Barnes clinic page
Book an Appointment
Booking an appointment with one of our therapists is quick and easy. There is no long waiting time and you don’t need a referral from your GP.