Understanding their significance following surgery to remove all or part of the prostate gland (prostatectomy).
The anatomy:
The pelvic floor muscles are muscles that attach to the pubic bone at the front and onto the back of your tail bone. These muscles are important in maintaining continence.
Voluntary contraction of the pelvic floor muscles will result in closure of the urethra (the tube where the urine leaves the body) preventing urine flow, thus helping to maintain continence.
It is also important to consider the urethral sphincters (the muscles surrounding the urethra) that control continence in men. The urethral sphincter is made up of smooth (involuntary) and skeletal (voluntary) muscle fibres. The smooth muscle fibres maintain continence without you having to think about it, this is called passive continence. The external urethral sphincter, made up of skeletal muscle, works with the pelvic floor muscles to maintain active continence.
Relevance to Prostatectomy:
Following a radical prostatectomy (removal of the prostate) urinary leakage is a commonly experienced. The risk of developing incontinence following radical prostatectomy can occur for many reasons. These include direct damage to the pelvic floor muscles, damage to the neural structures thus, decreasing the nerve supply to the muscles involved in maintaining continence, or injury to the urethral sphincters. Therefore, following surgery, urine leakage can be experienced during everyday tasks such as laughing, coughing or whilst exercising. This can be difficult for men and their families following surgery. Fortunately, symptoms of urinary incontinence improve over time and the evidence suggests that learning how to engage your pelvic floor muscles, and subsequent strengthening exercise also helps!
How can we help?
At the White Hart Clinic we have a pelvic floor physiotherapy service that will facilitate a quicker return to normal function. Prior to your radical prostatectomy a thorough pelvic floor assessment can be performed and your pelvic floor physiotherapist will educate you on correct activation of these muscles. Following the assessment, a personalised pelvic floor muscle training program will be implemented to suit your personal needs and goals. Further education on the surgery, post-operative recovery and good bladder habits are also likely to be discussed during your treatment.
For further queries please do not hesitate to contact us on 020 8876 9897 or email info@whitehartclinic.co.uk
References:
Anderson, C. A., Omar, M. I., Campbell, S. E., Hunter, K. F., Cody, J. D., & Glazener, C. M. (2015). Conservative management for postprostatectomy urinary incontinence. [Research Support, Non-U.S. Gov't]. Cochrane Database Syst Rev, 1, CD001843. doi: 10.1002/14651858.CD001843.pub5.
Hunter, K. F., Moore, K. N., Cody, D. J., & Glazener, C. M. (2004). Conservative management for postprostatectomy urinary incontinence. [Review]. Cochrane Database Syst Rev(2), CD001843. doi: 10.1002/14651858.CD001843.pub2
Koraitim, M. M. (2008). The male urethral sphincter complex revisited: an anatomical concept and its physiological correlate. [Review]. J Urol, 179(5), 1683-1689. doi: 10.1016/j.juro.2008.01.010
Walz, J., Burnett, A. L., Costello, A. J., Eastham, J. A., Graefen, M., Guillonneau, B., . . . Villers, A. (2010). A critical analysis of the current knowledge of surgical anatomy related to optimization of cancer control and preservation of continence and erection in candidates for radical prostatectomy. [Review]. Eur Urol, 57(2), 179-192. doi: 10.1016/j.eururo.2009.11.009
Lucas, M. G., Bosch, R. J., Burkhard, F. C., Cruz, F., Madden, T. B., Nambiar, A. K., . . . Pickard, R. S. (2012). EAU guidelines on assessment and nonsurgical management of urinary incontinence. [Practice Guideline]. Eur Urol, 62(6), 1130-1142. doi: 10.1016/j.eururo.2012.08.047
Goode, P. S., Burgio, K. L., Johnson, T. M., 2nd, Clay, O. J., Roth, D. L., Markland, A. D., . . . Lloyd, L. K. (2011). Behavioral therapy with or without biofeedback and pelvic floor electrical stimulation for persistent postprostatectomy incontinence: a randomized controlled trial. [Comparative Study Multicenter Study Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, U.S. Gov't, Non-P.H.S.]. JAMA, 305(2), 151-159. doi: 10.1001/jama.2010.1972
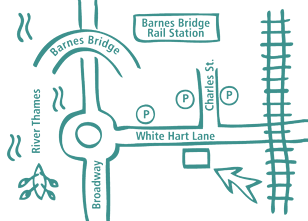
Our Barnes Clinic
Our clinic is located in Barnes, South-West London and is easily accessible by public transport.
For more information including parking and other practicalities see our Barnes clinic page
Book an Appointment
Booking an appointment with one of our therapists is quick and easy. There is no long waiting time and you don’t need a referral from your GP.