Stiff neck, nervous headache, stressed vagina? It’s not just the muscles in your shoulders that can knot with tension. We report on the physiotherapy that could save your sex life.
Tanith Carey | Published: 3 August 2014 | Sunday Times Style Magazine
Anna Martin had more reason than most brides to be nervous in the run-up to her big day. It was not just the rush to get everything ready for the ceremony. It was also the countdown to the wedding night and the pressing need to find out why sex with her fiancé was so painful. The discomfort was now so severe, they had not made love for a year.
“When I first met my husband, Hugh, through work five years ago, we had a normal, healthy sex life,” says Anna, 28, a professional cellist from St Albans. “Then, a year before the wedding, I started to feel a tightness in my pelvis and a burning sensation every time I went to the loo. When I did go, I hardly passed any urine.” What sounded like a routine bladder infection refused to go away, and after a few weeks the stinging was replaced by constant throbbing pain.
Anna says: “My whole genital area became sensitive to touch. It got so bad, it was impossible to sit for long periods or play the cello, so I couldn’t work either. It was hell. Sex was out of the question and at times my pain levels were 9 out of 10.”
In an effort to get to the root of the problem, Anna made several appointments with both her GP and her gynaecologist. When they found no evidence of an infection or an abnormal growth, she was told there was nothing to be done. She simply had to “learn to live with it”. The antidepressants prescribed to numb the nerve pain made little difference.
Desperate for answers, Anna trawled the internet and found a little-known, and surprising, solution: muscle-tension massage. This novel approach, imported from America, treats pelvic problems in the same way as neck, back or headache pain, with massage and physiotherapy.
Anna says: “Until that point, a physiotherapist was someone I associated with releasing frozen shoulders, but it seemed logical. I found a clinic in west London offering the treatment. When the physio examined me, she told me my vaginal muscles were rigid and my pelvic-floor muscles had tightened completely. She explained that while many people hold their tension in their neck and shoulders, others feel tension in their pelvic floor and hold the muscles up high all the time.”
In the rush to address the problem in time for her wedding the following spring, Anna had about 15 sessions. During the treatments, the physiotherapist used internal massage to work away the hypersensitive knots of tension. At home, Anna also did exercises to stretch out her hips, relaxing the muscles again, so that little by little she was able to reclaim her sex life.
This treatment may sound unorthodox, but Anna’s experience is not unique. Recent studies estimate that as many as one in four women will suffer chronic pelvic pain for more than six months at some time during their life. If the condition has no obvious cause, many women are told to go away and “have a glass of wine” because it’s purely psychological. But an increasing number of specialist women’s health physiotherapists — more than 700 are registered in the UK — are treating pelvic pain on the basis it has the same roots as tension in the upper body.
"I was too mortified to say anything, even to my partner. It was like I had a permanent disability no one could see."
Two pioneers of this approach, the American doctors David Wise and Rodney Anderson, point out that the area is made up of a dense muscular network that holds up the core of the body and protects organs such as the uterus, bladder and bowel. Under stress, the muscles get taut and tight, cutting off the blood and oxygen supply. Lactic acid builds up, and the nerves get irritated, causing pain that radiates out into the vagina, vulva and rectal area.
Injuries during birth or caused by forceps deliveries can also cause internal damage, leading to the organs and surrounding tissues becoming “twisted” and pulled out of place. According to the Expert Review of Obstetrics & Gynecology, symptoms often overlap and include vaginal pain, itching, cramps, muscle spasms, constipation, cystitis and incontinence. Sometimes pain is so severe that riding a bike, sitting for long periods or even walking are excruciating. And because these problems are difficult to talk about, and the anatomy looks normal, treating this area with massage is still a health taboo.
The result is a hidden epidemic that leaves tens of thousands of women in this country living a life of “quiet desperation”. Wise says: “Most people with pelvic pain think they have not met another person with a similar condition, even though millions of people suffer from it.”
Francesca Linstead, a 52-year-old radio producer from Teddington, also thought her pelvic pain was untreatable and, as a result, didn’t have sex for two years. The problem started when Francesca felt a tender lump in the inner wall of her vagina that made penetration difficult.
Her first fear was cancer, but when nothing was found, she was referred to an NHS women’s health physiotherapist at the Chelsea and Westminster Hospital in London. She traced the problem back to Francesca’s coil being fitted too roughly three years earlier.
“The insertion was so painful, I had to tell the doctor to stop,” Francesca says, “but afterwards I thought little of it. Over the years, it seems an area of muscle tension formed around the damaged tissue. Once sex started to hurt, the problems quickly got worse. The more discomfort I anticipated, the more I braced myself. I was too mortified to say anything, even to my partner. It was like I had a permanent disability no one could see.”
At first, Francesca admits, she had to overcome the “ick” factor: “It all sounded embarrassing, but the sessions were pleasantly businesslike. There was nothing pleasurable about them. At times the feeling of the physio’s gloved finger pressing on the rigid muscle of my vaginal wall was hard to take. But gradually, over several weeks, the golf-ball-sized lump shrank down to the size of a pea.”
Even though women are now able to get physiotherapy treatment on the NHS in some parts of the country, it seems that Britain is still lagging behind other nations. In France and Norway, every mother who has a vaginal delivery sees a physical therapist after giving birth to head off problems such as urinary incontinence or damaged pelvic-floor muscles.
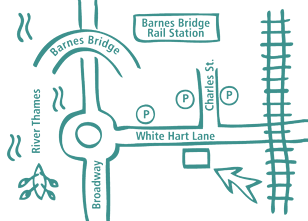
Christien Bird, a women’s health physiotherapist based at the White Hart Clinic in West London, says that, on average, women wait 10 years before they seek help. Treatment aims to be less clinical than in gynaecology practices, she adds. “Women are examined in a dimly lit room. There are no stirrups, white coats or speculums. We wear gloves and map a woman’s internal organs and locate the areas of pain.”
Although orgasm will relieve some pelvic tension, it only relaxes some of the muscles, says Bird. “When people have sexual dysfunction or pain, they usually can’t have an orgasm, so it’s not an option in the first place. Orgasm isn’t a magic cure, because there are so many other factors involved.”
After a year of treatment, Anna finally got the wedding night she had hoped for. “I was lucky, I recovered 100%. But it’s ironic in this sex-obsessed age that we are too squeamish to talk about this. It amazes me I couldn’t find the solution for so long, yet the explanation was so simple.”
For Francesca, the new approach was a “lifeline”, although ultimately her 10-year relationship didn’t survive the absence of sex.
“The intimacy was gone,” she says, “but I’m lucky to still have a second chance at a sex life. So many doctors still don’t seem to know this approach even exists. Think of all the other women out there who have to abandon making love and are seeing their relationships disintegrate as a result, because they don’t realise there’s a cure.”
whitehartclinic.co.uk
Image: Horacio Salvinas
Chartered Physiotherapists - see this blog post on the CSP website
Our Barnes Clinic
Our clinic is located in Barnes, South-West London and is easily accessible by public transport.
For more information including parking and other practicalities see our Barnes clinic page
Book an Appointment
Booking an appointment with one of our therapists is quick and easy. There is no long waiting time and you don’t need a referral from your GP.