To celebrate Back Care awareness week (October 7 – October 12) we are going to look at back pain. We will build on our previous blog post from March 2019 regarding triggers for low back pain; leading us into how this influences treatment based on the latest available evidence.
As our previous blog describes, physical causes are not the only triggers for back pain. Anxiety, depression, family and occupational stressors, and significant life events can trigger and affect prognosis for low back pain. Poor understanding of pain is also important to consider. From a physical causation standpoint, the research is moving away from the notion of poor lifting and posture as primary causes of back pain, and more so to inappropriate exposure to loading. This means either doing too much activity to soon or not having enough strength to tolerate your activity/occupation.
Regarding management, the research is continually supporting the following points of management for back pain:
Education and reassurance
This revolve around pain education and radiology. What we know is that pain is an alarm system and does not equal damage. This is particularly true in persistent and chronic cases of back pain. Education is vital to reduce fear of back pain and allows us to progress with your physical rehabilitation. Radiology is an important tool when used appropriately. Over 90% of low back pain cases are classed as non-specific, meaning no specific structure can be identified as the source of pain. This is further supported by studies have shown that “pathologies” such as disc prolapse, and arthritis are present even in those with no history of back pain. A careful clinical examination by your physio needs to be made to gain a clearer picture of your symptoms before radiology is used.
Progressive return to activity
This is individual to you, based on how your symptoms are impacting your day to day living, and your end goal for rehabilitation. Whether this is return to your daily activities, occupation or sport, a rehabilitation plan needs to be made. This starts as soon as possible. Even a couple of days of bed rest can impact muscular strength and endurance. Best advice is to keep moving in a capacity which you can manage, and build this day by day slowly, even with a small amount of pain. This includes stretching, gentle walking and daily activities as advised by your physiotherapist. Progression can then be made with a more structured exercise regime which can include a home exercise and or gym program to build your tolerance to your rehabilitation goal and build into your regular routine.
In Summary, what does this mean for your back pain?
Do not fear your back when you have back pain. It is still a strong and stable structure, 95% of all cases will improve with appropriate physiotherapy and exercise management. We must consider all triggers both physical and psychosocial (relating to the interrelation of social factors and individual thought and behaviour.) Treatment needs to be very individual, there is no recipe approach to beat back pain as every person has different goals for rehabilitation. It is also important that as health care professionals, we work together to achieve the best outcome for you.
Summary of Key points
- Contributors to back pain are not just physical, certain psychological components such as stress, anxiety, depression, social support & occupational satisfaction are strongly linked with prevalence and prognosis for low back pain.
- Pathological findings on imaging relate poorly to pain source and severity as these findings are often found in those without pain.
- Pain does not equal structural damage! We can move with acceptable levels of pain and be reassured we are not making things worse.
- Treatment of back pain must be related to your pain experience i.e. how it affects your daily life, what level of function you currently see yourself at and your goals for rehabilitation.
- Active treatment i.e. exercise must accompany all treatment for rehabilitation and prevent of low back pain.
Written by Rob Walsh, Physiotherapist
Our Barnes Clinic
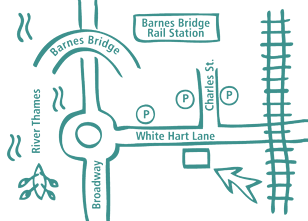
Our clinic is located in Barnes, South-West London and is easily accessible by public transport.
For more information including parking and other practicalities see our Barnes clinic page
Book an Appointment
Booking an appointment with one of our therapists is quick and easy. There is no long waiting time and you don’t need a referral from your GP.